High cholesterol: these are two words that many dread seeing on medical test results. Modern medicine contends that high cholesterol is linked to an increased risk of developing heart disease, which in turn increases risk of having a heart attack or stroke. Currently the most common treatment for high cholesterol is for your doctor to prescribe a medication from the class of drugs known as statins. There’s no doubt that statins measurably reduce cholesterol for some people. For the vast majority of doctors, even naturopathic ones, this is as far as they go. The risk of fatal heart attack or stroke is lessened, and that’s all that matters to them. But is this really a good approach to health? Patients given statin drugs to control cholesterol face taking them lifelong. and never get to the root of what’s going on inside their bodies. In Cellular Healing TV podcast episode 114, Meredith and I interview Dr. Jack Wolfson, author of “The Paleo Cardiologist: The Natural Way to Heart Health.” We discuss some of the myths still being spread about heart health. The notion that cholesterol is bad and that statins are necessary to control cholesterol levels are two big ones.
What is Cholesterol?
Cholesterol is simply a fatty substance found in every single cell in your body, both in the cell membranes and within organelles inside the cell. Cholesterol is a vital substance, necessary for numerous functions, including:
- Maintaining cell membrane integrity and fluidity within the cell
- Assisting with cell signaling
- Integral for hormone production, especially reproductive hormones
- Vitamin D production
- Used in bile acids production, necessary for digestion
- Brain and neurological function (the brain generally holds about 25% of the body’s cholesterol)
Cholesterol is so vital to the body’s functions that your liver can make all that it needs to survive. It’s not reliant upon you to eat cholesterol to provide the necessary amount, though some of the cholesterol that you eat may make its way into the bloodstream. Looking at the importance of cholesterol, it’s difficult to imagine how modern medicine has come to vilify it. The answer to that involves a look at the plaque inside of hardened arteries (atherosclerosis).
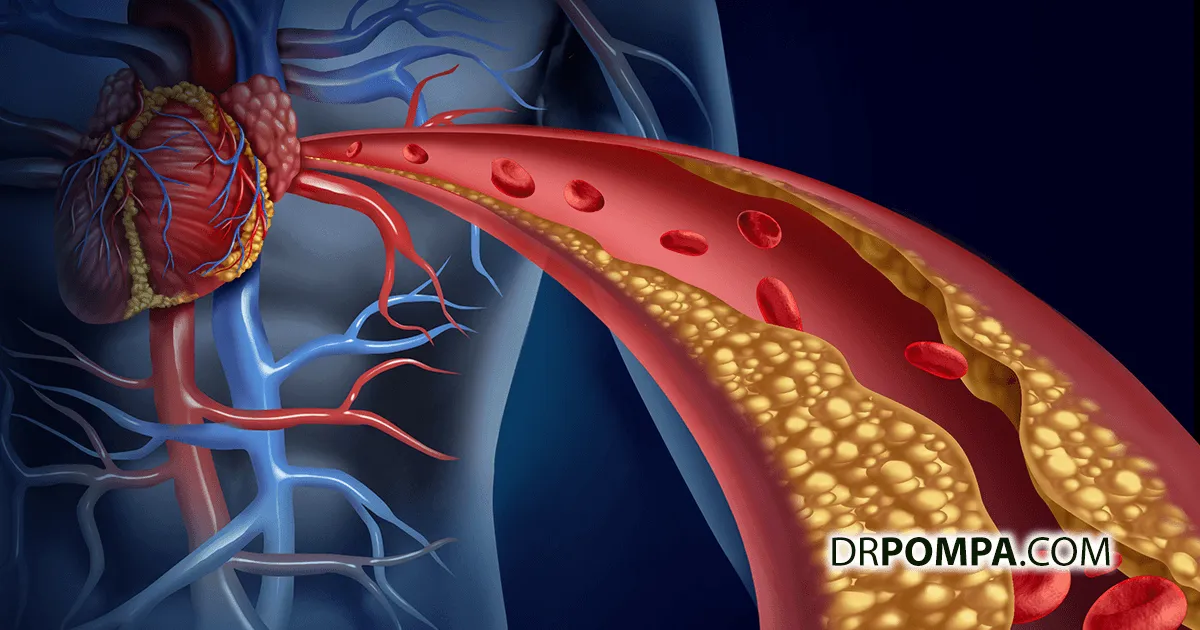
We know that heart disease arises from hardened arteries, called atherosclerosis. In those with atherosclerosis, plaque builds up along arterial walls, diminishing both the elasticity of the artery and the space available for blood to flow through it. When doctors analyzed the plaque itself, they found that it was made up of several components, including calcium and, you guessed it, cholesterol. This led to cholesterol eventually being declared dangerous at high levels in the blood, and the development of drugs to lower cholesterol, like statins.
When looking at cholesterol levels, doctors further subdivide it into LDL (low density lipoproteins), HDL (high density lipoproteins), and triglycerides (not actually a cholesterol, but another kind of blood fat, involved in energy storage). A lipid panel is the usual test for establishing blood cholesterol levels, and measures total cholesterol in the blood. The results are compared against a range of norms for each type. Depending on where you fall compared to these “normal” ranges, your doctor could advise the use of statins and/or a “heart healthy” low fat diet.
Learn more about cholesterol sulfate and the dangers of glyphosate here.
Cholesterol can’t travel alone through the blood, because it’s water insoluble. Once it’s manufactured in the liver, cholesterol is combined with other compounds like sulfur or protein to transit through the bloodstream. The protein in a lipoprotein surrounds the cholesterol kind of like passengers in a car, hence the word lipoprotein. LDL (low density lipoprotein) is considered the bad cholesterol, the most involved in damage to the inner walls of blood vessels. In actuality, LDL isn’t necessarily a bad thing. It’s sent out from the liver to perform the many functions that cholesterol performs, as noted. HDL (high density lipoprotein) is in many ways LDL’s balance. HDL’s are on their way back to the liver, and are involved in healing damage to vessel walls (plaque removal) and latching on to spent or oxidized LDL particles in order to return them to the liver for reprocessing. This is why HDL is considered the good cholesterol. HDL levels are what doctors are looking for when they test total cholesterol. Statins come in when doctors want to lower LDL levels in the blood.
How Do Statins Work?
Statins are basically enzyme blockers. They target a reductase enzyme, specifically HMG-CoA reductase (abbreviated to HMGCR), which sends the trigger to the liver to produce cholesterol. Normally this process happens naturally in the body, and is balanced by other triggers, which induce the liver to break down LDL particles. Statins inhibit HMGCR production, which reduces the amount of cholesterol that the liver can produce, often resulting in lowered total blood cholesterol. Sounds good, right? Here’s the catch…
Mainstream doctors will tell you that high cholesterol will increase your risk of heart attack or stroke, and so, therefore, taking a lipid lowering drug like a statin will reduce that risk. Then they use the standard lipid panel to determine cholesterol levels, and a whole lot of people end up on statin drugs. But did you know that many people who have heart attacks don’t have high cholesterol levels? A very large study using data from the WHO established that only about half of the people who suffered from a heart attack had elevated LDL levels at the time. About 20% of those in the study were taking lipid lowering meds and still had a heart attack. This calls the effectiveness of statin drugs into question.
Now let’s look at the side effects of statins. We learned earlier that cholesterol is vital to the proper functioning of our cells and numerous systems of the body. Inhibiting the production of cholesterol can have some very negative effects, and we see this borne out in the listed side effects of statin drugs which include:
- Myalgia (muscle pain or weakness) and muscle damage, potentially severe
- Insomnia
- Headaches
- Rashes
- Digestion problems
- High blood pressure
- Type 2 diabetes (increased risk)
- Neurological problems, including memory loss, brain fog, mental confusion, cognition problems
Now, scroll back to the top of the article where I listed a few of cholesterol’s vital functions in the body. Can you see the connection? A lot of these side effects are exactly what could happen in a body with a reduced ability to produce cholesterol. That’s what statins do.
A Better Solution to High Cholesterol
The problem with modern medicine’s approach to balancing cholesterol levels is really the same problem that we see time and again in mainstream medical practice: it doesn’t get to the underlying cause (R1). Be sure to listen to our podcast with Dr. Wolfson where we go into detail on what we believe to be the true cause behind LDL build-up in the blood. If inflammation and toxicity came to mind, then you’re on the right track.
I’ve spoken and written about inflammation countless times because it’s vital to understand the relationship between cellular inflammation and malfunction in the body. There certainly is a connection between LDL levels in the blood and arterial damage, but doctors aren’t testing properly or offering treatments that can help you get well.
To illustrate the importance of the right tests for cholesterol, and the right way to be thinking of LDL/HDL levels, review this short, classic video.
I described the lipoprotein as a car with the cholesterol as the passengers inside the car. The number of passengers determines the density of the lipoprotein (the car). Imagine that your blood is a highway, and that there’s a traffic jam. What matters more in clearing the traffic jam, the number of cars on the highway, or the number of passengers in each car? It’s the number of cars on the highway, and their size, that matters more in establishing cholesterol levels and inflammatory damage to the blood vessel walls. That’s the number you need, and what must be evaluated to determine what steps to take to decrease that inflammation.
Once you know those numbers you can begin to use natural methods and a Multi-Therapeutic Approach to bring your cells back to health, and reduce the factors that led to the inflammation in the first place. Remember, just because you have high cholesterol doesn’t mean you are at risk for a heart attack, just as having low cholesterol doesn’t mean you aren’t at risk. Fix the cell, get well. I can’t tell you get off statins, only your doctor can do so. I can suggest you educate yourself about statins, cholesterol’s true function, inflammation, and root causes of disease.
- CHTV Episode 114: The Truth About Statin Drugs and Cholesterol
- R1: Removing the Source of Toxins
- The Dangers of Glyphosate: An Interview with Dr. Stephanie Seneff
- Dr. Pompa's Top Sleep and Anxiety Strategies
- R4: Reducing Cellular Inflammation
- PompaCore Cellular Detox™ – A Top 5 Strategy to Create Your Best Health Ever
- My Multi Therapeutic Approach
- Detox Your Life: My Toxic Top 10
- Sachdeva, Amit, MD, Christopher P. Cannon, MD, Prakash C. Deedwania, MD, Kenneth A. LaBresh, MD, Sidney C. Smith, Jr., MD, David Dai, MS, Adrian Hernadez, MD, and Gregg C. Fonarow, MD. “Lipid levels in patients hospitalized with coronary artery disease: An analysis of 136,905 hospitalizations in Get With The Guidelines.” AHJ – American Heart Journal. January 2009. http://www.sciencedirect.com/science/article/pii/S0002870308007175.