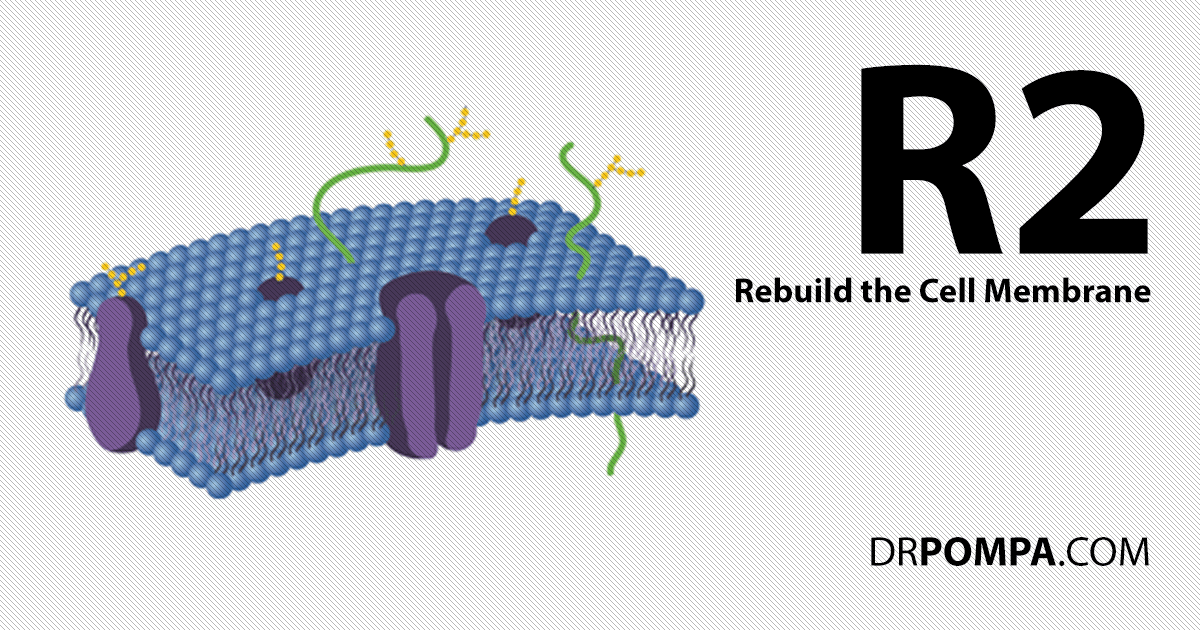
R2 – Regenerating The Cellular Membrane
The cell membrane or lipid bilayer, which surrounds every cell in our body, acts as a protective barrier and controls what goes in and out of the cell. In order for our cells to effectively eliminate toxins, they must have a healthy and functional membrane.1
Embedded within the cell membrane are various types of proteins that act as receptors, channels, pumps, and enzymes. These proteins are responsible for receiving signals from the cell's environment, transporting substances in and out of the cell, and facilitating chemical reactions within the cell.2
For example, when a hormone binds to its specific receptor on the cellular membrane, it triggers a series of events that ultimately lead to a response from the cell. This response can range from changes in gene expression to altering the cell's shape and movement.3
Similarly, ion channels in the cellular membrane help maintain the cell's internal environment by regulating the flow of ions such as sodium, potassium, and calcium. This is important for functions like muscle contraction and nerve signaling.4
When everything is in balance, this system works like a well-oiled machine. However, when cellular inflammation is present, it impedes the function of membrane proteins. In order to regenerate the cellular membrane back to ideal form, toxins that cause inflammation must be eliminated.5
If you haven’t already, read more about R1 – removing the source of toxins that cause inflammation.
What Causes Cellular Membrane Inflammation?
Cellular membrane inflammation occurs when toxins such as heavy metals, mold, and hidden infections cause damage to the cellular membrane. When toxins breach this barrier, they disrupt essential processes within the cell, leading to inflammation. This inflammation contributes to various health issues, including allergies, autoimmune diseases, and hormone dysfunction.6
An Inflamed Cellular Membrane Affects Integral Membrane Proteins
One aspect that is affected by an inflamed cellular membrane is integral membrane proteins (IMP). These are specialized protein molecules that are embedded within the cellular membrane. They play crucial roles in cell signaling, transport of molecules, and maintaining the structural integrity of the cell.7
When the cellular membrane is inflamed, it disrupts the function and structure of integral membrane proteins. This is because inflammation causes changes in the composition and fluidity of the cellular membrane, which alters the positioning and conformation of IMPs. As a result, their ability to perform essential functions is compromised.8
Moreover, inflamed cellular membranes also lead to increased permeability, allowing molecules that are typically not allowed to enter the cell to pass through. This is dangerous as it allows harmful substances or pathogens to enter the cell and cause damage.9

Cellular Membrane Inflammation Reduces Transport Into And Out Of The Cell
When there is inflammation throughout the cellular membrane, it leads to nutrient deficiencies. This is because the cellular membrane regulates the passage of nutrients and other molecules into and out of the cell. Essential vitamins and minerals are not able to enter the cell properly, resulting in inadequate nutrition for cellular metabolism.
An inflamed membrane also causes difficulty in removing waste products from the cells. This leads to a buildup of toxins and metabolic waste, further exacerbating the inflammation. As a result, cells are not able to function optimally, leading to tissue damage and various health issues.10
Inflammation of cellular membranes also affects cell signaling and communication. This is because cellular membranes play a crucial role in transmitting signals between cells and organ systems. When inflamed, these signals are not effectively transmitted, leading to disruptions in normal body functions.11
Furthermore, chronic inflammation of cellular membranes is known to contribute to the development of certain diseases and conditions such as atherosclerosis, rheumatoid arthritis, and various autoimmune disorders. It has also been linked to premature aging and increased risk of chronic diseases.12 13
Dr. Bruce Lipton’s Discovery Between Innate Intelligence And The Cellular Membrane
Dr. Bruce Lipton is a well-known cellular biologist who has been studying the effects of the cell membrane on gene expression for decades. His groundbreaking research has challenged traditional notions of genetic determinism and shed light on how our environment and perceptions affect the expression of our genes.
One of Lipton's key findings is that the cell membrane is not just a protective barrier but also acts as an intelligent interface between the cell and its external environment. This means that the signals from our environment can directly influence the behavior of our cells.14
At the core of Lipton's research is the concept of epigenetics, which refers to changes in gene expression without any alteration in the underlying DNA sequence. He has shown that the cell membrane is responsible for controlling which genes are turned on or off, and this can be influenced by various environmental factors such as nutrition, stress, and emotions.15
Lipton's research dictates that our perceptions and beliefs can override genetic predispositions and have a significant impact on our health and well-being. For example, stress and negative emotions lead to changes in the cell membrane, which affect gene expression. This means that our thoughts, attitudes, and perceptions directly influence our biology at the cellular level.
Simply put, positive emotions and a healthy environment help to keep the cell membrane in an optimal state, promoting the expression of beneficial genes.
A Dysfunctional Cellular Membrane Leads To Undesirable Gene Expression
When the cellular membrane becomes dysfunctional, it affects the signaling pathways that control gene expression. These pathways rely on specific molecules called signaling molecules to communicate with the cell's nucleus and activate or suppress certain genes. If the cellular membrane is compromised, these signaling molecules are not able to properly reach their intended target, resulting in altered gene expression.16
A dysfunctional cellular membrane leads to oxidative stress, which is an imbalance between the production of reactive oxygen species (ROS) and the body's ability to detoxify them. Oxidative stress damages DNA and epigenetic modifications, resulting in changes in gene expression.17
This is why regenerating the cellular membrane to an ideal state is so foundationally important to achieving good health. A properly functioning cellular membrane initiates the cell to turn on good genes and turn off bad genes, ensuring your best genetic traits are expressed.
Regenerating The Mitochondrial Membrane – ATP Energy Is Required To Detox The Cell
Mitochondria are known as the powerhouse of our cells, responsible for generating ATP (adenosine triphosphate), which is the main source of cellular energy. However, when the mitochondrial membrane becomes inflamed, it disrupts the normal functioning of mitochondria and leads to a decrease in energy production.18
To prevent this, it is important to understand the causes of mitochondrial membrane inflammation and how we can reduce it. One of the main causes is oxidative stress. Antioxidants help neutralize these free radicals, protecting the mitochondrial membrane from inflammation.19
Another factor that contributes to mitochondrial membrane inflammation is a high sugar and processed food diet. These types of foods result in oxidative stress and also lead to insulin resistance, which can further damage the mitochondria. It is important to maintain a balanced and healthy diet to support optimal mitochondrial function.20
In addition to reducing inflammation, it is important to support the repair and regeneration of the mitochondrial membrane. This can be done through exercise, specifically HIIT exercise, which has been shown to improve mitochondrial function and reduce inflammation in the body.21

The Process Of Regenerating The Cellular Membrane
In a process called lipid synthesis, the cell is able to produce new phospholipids and incorporate them into the damaged membrane. This process involves enzymes and other proteins that work together to build the phospholipids from smaller molecules such as fatty acids. The newly synthesized lipids are then transported to the site of damage in the membrane where they can seamlessly integrate and repair any gaps or ruptures.22
The Composition Of The Cellular Membrane
Omega-6 and omega-3 fatty acids play important roles in maintaining the fluidity and permeability of the cellular membrane. Omega-6 and omega-3 are both polyunsaturated fatty acids (PUFAs), meaning they have multiple double bonds in their chemical structure. These fatty acids cannot be produced by our bodies and must be obtained through our diet.23
The balance between these two types of fats is crucial for the proper functioning of the cellular membrane. Too much omega-6 fatty acids in proportion to omega-3 can lead to increased inflammation and decreased fluidity of the membrane. This can affect the ability of substances to pass through the membrane and disrupt important cellular processes.24
On the other hand, the proper proportion of omega-3 fatty acids can improve the fluidity of the membrane and regulate inflammatory responses, leading to better overall health. Studies have also shown that the consumption of adequate amounts of omega-3 fatty acids improve cell signaling and communication.25
The traditional Western diet tends to be high in omega-6 fatty acids due to the widespread consumption of processed foods and vegetable oils. However, research has shown that an imbalanced ratio of omega-6 to omega-3 can increase the risk of chronic diseases. Even worse, processed vegetable oils often contain rancid omega-6 fatty acids. Consuming rancid omega-6 oils are linked with chronic inflammation and a long list of diseases.26 27
What Diet Provides High Quality Omega-6 And Omega-3 Fatty Acids?
High Quality Omega-3 Fatty Acid Foods
Consuming whole, unprocessed foods with sources of omega-3 fatty acids into our diet, such as fatty fish like salmon, sardines, and mackerel, as well as plant-based sources like chia seeds, flaxseeds, and walnuts are essential for cellular membrane function.28
High Quality Omega-6 Fatty Acid Foods
Nuts and seeds are excellent sources of omega-6 fatty acids. Some of the best options include walnuts, almonds, pumpkin seeds, and sunflower seeds. These foods not only provide omega-6 fatty acids, but also contain other beneficial nutrients like fiber, protein, and antioxidants.29
Avocado is another great source of omega-6 fatty acids. In addition to providing healthy fats, avocados also contain vitamins, minerals, and antioxidants that support heart health and reduce inflammation.30
Olive oil is a staple in the Mediterranean diet and is known for its many health benefits. It is a good source of omega-6 fatty acids, as well as monounsaturated fats which have been linked to improved heart health.31
Grass-fed meat is a great source of omega-6 fatty acids, as well as other important nutrients like protein and iron. Grass-fed meat also contains high quantities of conjugated linoleic acid (CLA) which helps us build muscle and burn fat.32 33
Flaxseeds are an excellent plant-based source of omega-6 fatty acids. They also contain high levels of fiber and antioxidants, making them a nutritious addition to any diet. Similar to flaxseeds, chia seeds are also a great plant-based source of omega-6 fatty acids.34

Regenerating The Cellular Membrane With My Cellular Healing Diet
My Cellular Healing Diet provides the body with the products required to repair the lipid bilayer like healthy omega-6 and omega-3 fatty acids from real, whole foods. By incorporating a diet with the build blocks for cellular membrane repair, the body systemically regenerates cellular membranes.
Simply put, if we remove the toxins presented in R1 and provide the building blocks for R2 – Regenerating The Cellular Membrane, the body is able to heal itself.
Now it is time for R3 – Restoring Cellular Energy.
References
1 Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. The Lipid Bilayer. Available from: https://www.ncbi.nlm.nih.gov/books/NBK26871/
2 Qiu W, Fu Z, Xu GG, Grassucci RA, Zhang Y, Frank J, Hendrickson WA, Guo Y. Structure and activity of lipid bilayer within a membrane-protein transporter. Proc Natl Acad Sci U S A. 2018 Dec 18;115(51):12985-12990. doi: 10.1073/pnas.1812526115. Epub 2018 Dec 3. PMID: 30509977; PMCID: PMC6304963.
3 Robertson JL. The lipid bilayer membrane and its protein constituents. J Gen Physiol. 2018 Nov 5;150(11):1472-1483. doi: 10.1085/jgp.201812153. Epub 2018 Sep 25. PMID: 30254021; PMCID: PMC6219687.
4 Levitan I, Fang Y, Rosenhouse-Dantsker A, Romanenko V. Cholesterol and ion channels. Subcell Biochem. 2010;51:509-49. doi: 10.1007/978-90-481-8622-8_19. PMID: 20213557; PMCID: PMC2895485.
5 Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L. Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017 Dec 14;9(6):7204-7218. doi: 10.18632/oncotarget.23208. PMID: 29467962; PMCID: PMC5805548.
6 Langan D, Rose NR, Moudgil KD. Common innate pathways to autoimmune disease. Clin Immunol. 2020 Mar;212:108361. doi: 10.1016/j.clim.2020.108361. Epub 2020 Feb 10. PMID: 32058071; PMCID: PMC8324042.
7 Majeed S, Ahmad AB, Sehar U, Georgieva ER. Lipid Membrane Mimetics in Functional and Structural Studies of Integral Membrane Proteins. Membranes (Basel). 2021 Sep 3;11(9):685. doi: 10.3390/membranes11090685. PMID: 34564502; PMCID: PMC8470526.
8 de Groot NS, Burgas MT. Is membrane homeostasis the missing link between inflammation and neurodegenerative diseases? Cell Mol Life Sci. 2015 Dec;72(24):4795-805. doi: 10.1007/s00018-015-2038-4. Epub 2015 Sep 24. PMID: 26403788; PMCID: PMC5005413.
9 Bednarek R. In Vitro Methods for Measuring the Permeability of Cell Monolayers. Methods Protoc. 2022 Feb 9;5(1):17. doi: 10.3390/mps5010017. PMID: 35200533; PMCID: PMC8874757.
10 Ammendolia, D.A., Bement, W.M. & Brumell, J.H. Plasma membrane integrity: implications for health and disease. BMC Biol 19, 71 (2021). https://doi.org/10.1186/s12915-021-00972-y
11 Bender EC, Kraynak CA, Huang W, Suggs LJ. Cell-Inspired Biomaterials for Modulating Inflammation. Tissue Eng Part B Rev. 2022 Apr;28(2):279-294. doi: 10.1089/ten.TEB.2020.0276. Epub 2021 Jul 29. PMID: 33528306; PMCID: PMC9063153.
12 Duan L, Rao X, Sigdel KR. Regulation of Inflammation in Autoimmune Disease. J Immunol Res. 2019 Feb 28;2019:7403796. doi: 10.1155/2019/7403796. PMID: 30944837; PMCID: PMC6421792.
13 Pahwa R, Goyal A, Jialal I. Chronic Inflammation. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493173/
14 Gustafson C. Bruce Lipton, PhD: The Jump From Cell Culture to Consciousness. Integr Med (Encinitas). 2017 Dec;16(6):44-50. PMID: 30936816; PMCID: PMC6438088.
15 Virgallito, L. (2021, November 30). How our thoughts control our DNA. Bruce H. Lipton, PhD. https://www.brucelipton.com/how-our-thoughts-control-our-dna/
16 Smith M, Flodman PL. Expanded Insights Into Mechanisms of Gene Expression and Disease Related Disruptions. Front Mol Biosci. 2018 Nov 27;5:101. doi: 10.3389/fmolb.2018.00101. PMID: 30542652; PMCID: PMC6277798.
17 Juan CA, Pérez de la Lastra JM, Plou FJ, Pérez-Lebeña E. The Chemistry of Reactive Oxygen Species (ROS) Revisited: Outlining Their Role in Biological Macromolecules (DNA, Lipids and Proteins) and Induced Pathologies. Int J Mol Sci. 2021 Apr 28;22(9):4642. doi: 10.3390/ijms22094642. PMID: 33924958; PMCID: PMC8125527.
18 Cojocaru KA, Luchian I, Goriuc A, Antoci LM, Ciobanu CG, Popescu R, Vlad CE, Blaj M, Foia LG. Mitochondrial Dysfunction, Oxidative Stress, and Therapeutic Strategies in Diabetes, Obesity, and Cardiovascular Disease. Antioxidants (Basel). 2023 Mar 7;12(3):658. doi: 10.3390/antiox12030658. PMID: 36978905; PMCID: PMC10045078.
19 Huang ML, Chiang S, Kalinowski DS, Bae DH, Sahni S, Richardson DR. The Role of the Antioxidant Response in Mitochondrial Dysfunction in Degenerative Diseases: Cross-Talk between Antioxidant Defense, Autophagy, and Apoptosis. Oxid Med Cell Longev. 2019 Apr 7;2019:6392763. doi: 10.1155/2019/6392763. PMID: 31057691; PMCID: PMC6476015.
20 Kyriazis ID, Vassi E, Alvanou M, Angelakis C, Skaperda Z, Tekos F, Garikipati VNS, Spandidos DA, Kouretas D. The impact of diet upon mitochondrial physiology (Review). Int J Mol Med. 2022 Nov;50(5):135. doi: 10.3892/ijmm.2022.5191. Epub 2022 Sep 21. PMID: 36129147; PMCID: PMC9542544.
21 Chou CH, Fu TC, Tsai HH, Hsu CC, Wang CH, Wang JS. High-intensity interval training enhances mitochondrial bioenergetics of platelets in patients with heart failure. Int J Cardiol. 2019 Jan 1;274:214-220. doi: 10.1016/j.ijcard.2018.07.104. Epub 2018 Jul 27. PMID: 30072155.
22 Cockcroft S. Mammalian lipids: structure, synthesis and function. Essays Biochem. 2021 Nov 2;65(5):813-845. doi: 10.1042/EBC20200067. PMID: 34415021; PMCID: PMC8578989.
23 Fuentes NR, Kim E, Fan YY, Chapkin RS. Omega-3 fatty acids, membrane remodeling and cancer prevention. Mol Aspects Med. 2018 Dec;64:79-91. doi: 10.1016/j.mam.2018.04.001. Epub 2018 Apr 12. PMID: 29627343; PMCID: PMC6185832.
24 Cotogni P, Muzio G, Trombetta A, Ranieri VM, Canuto RA. Impact of the omega-3 to omega-6 polyunsaturated fatty acid ratio on cytokine release in human alveolar cells. JPEN J Parenter Enteral Nutr. 2011 Jan;35(1):114-21. doi: 10.1177/0148607110372392. PMID: 21224438.
25 Valentine RC, Valentine DL. Omega-3 fatty acids in cellular membranes: a unified concept. Prog Lipid Res. 2004 Sep;43(5):383-402. doi: 10.1016/j.plipres.2004.05.004. PMID: 15458813.
26 Patterson E, Wall R, Fitzgerald GF, Ross RP, Stanton C. Health implications of high dietary omega-6 polyunsaturated Fatty acids. J Nutr Metab. 2012;2012:539426. doi: 10.1155/2012/539426. Epub 2012 Apr 5. PMID: 22570770; PMCID: PMC3335257.
27 DiNicolantonio JJ, O'Keefe JH. Omega-6 vegetable oils as a driver of coronary heart disease: the oxidized linoleic acid hypothesis. Open Heart. 2018 Sep 26;5(2):e000898. doi: 10.1136/openhrt-2018-000898. PMID: 30364556; PMCID: PMC6196963.
28 Innes JK, Calder PC. Marine Omega-3 (N-3) Fatty Acids for Cardiovascular Health: An Update for 2020. Int J Mol Sci. 2020 Feb 18;21(4):1362. doi: 10.3390/ijms21041362. PMID: 32085487; PMCID: PMC7072971.
29 DiNicolantonio JJ, O'Keefe J. The Importance of Maintaining a Low Omega-6/Omega-3 Ratio for Reducing the Risk of Autoimmune Diseases, Asthma, and Allergies. Mo Med. 2021 Sep-Oct;118(5):453-459. PMID: 34658440; PMCID: PMC8504498.
30 Dreher ML, Davenport AJ. Hass avocado composition and potential health effects. Crit Rev Food Sci Nutr. 2013;53(7):738-50. doi: 10.1080/10408398.2011.556759. PMID: 23638933; PMCID: PMC3664913.
31 Schwingshackl L, Hoffmann G. Monounsaturated fatty acids, olive oil and health status: a systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014 Oct 1;13:154. doi: 10.1186/1476-511X-13-154. PMID: 25274026; PMCID: PMC4198773.
32 Nogoy KMC, Sun B, Shin S, Lee Y, Zi Li X, Choi SH, Park S. Fatty Acid Composition of Grain- and Grass-Fed Beef and Their Nutritional Value and Health Implication. Food Sci Anim Resour. 2022 Jan;42(1):18-33. doi: 10.5851/kosfa.2021.e73. Epub 2022 Jan 1. PMID: 35028571; PMCID: PMC8728510.
33 Daley CA, Abbott A, Doyle PS, Nader GA, Larson S. A review of fatty acid profiles and antioxidant content in grass-fed and grain-fed beef. Nutr J. 2010 Mar 10;9:10. doi: 10.1186/1475-2891-9-10. PMID: 20219103; PMCID: PMC2846864.
34 Parikh M, Maddaford TG, Austria JA, Aliani M, Netticadan T, Pierce GN. Dietary Flaxseed as a Strategy for Improving Human Health. Nutrients. 2019 May 25;11(5):1171. doi: 10.3390/nu11051171. PMID: 31130604; PMCID: PMC6567199.